
Written by Maria Bengtsson Lenn, journalist, doula, author of two books on pregnancy and child birth (in Swedish) and co-founder of the empowering community Own Your Birth (https://www.ownyourbirth.se/
Sitting in front of Dr. Bason-Mitchell, I wonder whether I should laugh or cry. My newly assigned OBGYN made on joke after the other, I guess in an attempt to lighten up the atmosphere in her grey, sterile office. As I put my legs in the cold stirrups for my first prenatal examination, a subtle, yet distinct door of disinfectants lingering in the air interrupted my thought process.
When she was done and my mind was back to my normal self, I remembered to ask her about the hospital’s flexibility during childbirth. “Every woman more or less ends up on their backs and begs for pain-relief anyway,” she replied.
Hand in hand, my husband Josh and I walked out of the hospital building on California Street in the Richmond District, excited about the little life we had created, but at the same time frightened by our “comedian” doctor and the rigid medical system we just had become part of. As a first-time mom I didn’t know what to expect, but a gut feeling told med that this was not what I wanted.
In the weeks following the visit, I thought a lot about the phrases “doctors deliver babies” and “midwives catch them,” or even better “midwives guide the mother or father to catch their own baby.” What consequences would these different expressions practised mean to us? What would be our role and how would that affect the way our baby entered the world?
After some extensive research on childbirth*, I realized that I was not willing to give my body and baby in the hands of doctors who are thought to look at childbirth as a problem that needs to be solved. After a few dialogues with my encouraging husband, I decided that I was going to give birth on my own terms, at my own pace and space. We were going to have a home birth.
Despite fearful comments from some of my own family members and the general distrust of natural birth from society, I dealt with it and entered the ninth month prepared both mentally and physically for a home birth. After my decision I called different midwives, and after my second interview I knew I had hit home. Circle of Life was our choice. The three midwives in the group all had an impressive history within midwifery, and the wise and spiritual ambiance in the little purple house in Fairfax, Marin, made each prenatal visit pure bliss.
In order to be admitted into Marin General in case of a necessary transfer during birth, I had to go to their clinic for checkups. The pace was fast and it felt very impersonal. To make sure a doctor wouldn’t “deliver me” in case of an emergency, I was able to see nurse-midwives; however they were over-worked and exhausted so that seeing them didn’t make me feel much different from my first appointment.
A sharp sensation grabbing hold of my lower back and belly woke me up around 5 am on Monday morning of April 3rd, 2005. Light contractions had come and gone through the last month so I wasn’t sure what to expect, but when the second one grasped me without much of a break in between, I got a clue. I walked into the bathroom, put a watch around my wrist and started to count the intervals of the contractions.

I wanted to let Josh sleep a little longer, so I went back to bed, closely observing my clock and trying to breathe through the now consistent waves of contractions that bobbed within my body. I closed my eyes and tried to remember Susan Brandford’s voice, “ Trust you body, women have given birth for millions of years; you know how to do it. “Surrender” became my mantra.
Every Thursday night in February and March, Josh and I, and six other couples, sat in a half moon circle learning and practising different pain coping techniques such as relaxed breathing and visualisations and movements that Susan Bradford, a doula and holistic childbirth educator, was teaching us. Bradford shed light on different birth options and weighed the pros and cons for each one. She didn’t try to underpin the fact that cesarean sections are sometimes necessary and save lives, and that epidurals can be a great pain relief when the process is long and the woman is exhausted. But she encouraged us to go natural as long as possible because both the women and the baby need to be fully conscious and able to physically respond to the different phases of labor in order to get the ultimate birth experience. Leopi Nicola, a licensed and certified midwife who was the primary midwife at our birth, agrees with Bradford and says that an epidural relaxes the pelvic region in women’s bodies making it both difficult for the baby to do the turns it has to do in order to come out and harder for the woman to push.
Another consequence is that the woman becomes more physically passive during birth when mobility is needed to help progress labor. Synthetic pitocin, which is widely used to induce labor, is often given with an epidural because the contractions that pitocin activates are so much more painful than natural contractions. All these different factors, just to mention a few, play an important role in the increasing rates of emergency cesareans and of other kinds of interventions and birth complications.
I woke up hearing giggles. My husband, Leopi and Joan, the second midwife who had just arrived, were entertained by watching my head fall toward the water in the birthing tub, when a new contraction got me up on my knees again. Because I hadn’t interrupted the physiological birth process with pitocin or drugs normally used in childbirth, my own body was producing the calming love hormone oxytocin, as well as the natural anaesthesia called endorphins—and I was high.
It had been about 40 hours since I first started counting the length of my contractions. Leopi came to our house a few hours after we’d called her in the morning; she didn’t rush because she could tell from the way I described my contractions that time was not yet ripe. Meanwhile, Josh and I went for the slowest walk in my life. I stopped every few minutes to breath through a contraction and felt as if I were going to have the baby right there on the street. When Leopi finally arrived she examined me and said that I was only one centimeter dilated and that I could be days away from having a baby. She encouraged me to get some rest, which proved to be impossible except for the minutes in between the contractions at the end of the night.
My power naps must have helped because once I was up that Tuesday morning there was no stopping me. I tried to be as active as I could in the hopes of being able to speed up the process. None of my efforts had helped. I hadn’t dilated more than three centimeters, when Leopi came back that afternoon. I was disappointed, but tried to keep my spirits up. Many hours later, when I still wasn’t progressing much, I started to feel uneasy. Leopi, who strongly believes in the force of the unconscious, asked if I had any fears that stopped me from letting go. I didn’t have to think long. The nurse-midwives at the other clinic had told me that I had scar tissue on my cervix, which would make my labor long and difficult, and now when there was no end in sight I started to doubt myself. Ultimately, I was scared to end up in the hospital, having a c-section. She countered my fears with love and trust, and told me that she could break the bag of waters (the amniotic sac) so that the labor would speed up, but if it didn’t and I got too exhausted, the last resort would be to go to the hospital. I couldn’t imagine it getting any more intense, so I said yes.
I lay down on my bed and as she was about to check me, another contraction came upon me. It was unbearable to lie on my back; my whole being screamed that I had to get up. Leopi waited patiently, but in hospitals around the world doctors and midwives are not always as understanding. Women have been encouraged, and in the past also forced, to lie on their backs throughout labor. IV fluids, epidurals, electronic fetal monitoring, and other interventional procedures conveniently disable women from following their instincts and being physically active during birth, making it easier for the hospital staff to do that they “have to” do.
My water broke soon after Leopi had broken the membrane, and I transitioned. Josh remembers it well: “You walked into the bathroom, faced a few contractions by yourself, and when you came out you had a different look on your face. You had become a birth warrior.”
It felt as if the primal animal within me had woken up when what I had feared the most was revealed. Instead of trying to control my breathing, I dove into the waves of the intenseness that overtook my body every few minutes. I had entered a different state of being—I wasn’t in my mind any more. I was fully present and I let my body do what it instinctively knew how to do. I finally dared to surrender.
My hands in tight grips around Josh’s slippery thighs, I arched like a cat animal and moaned along to the African drums playing in the background. It was 11 pm and my body was finally ready and my baby was on its way through the birth canal. We kissed and laughed in between the contractions. When I started to feel the urge to push I was excited. Finally, I could help my hard working baby with all my force. I pushed and pushed, stopped and panted for a short while so that I wouldn’t tear too much, but my baby wanted out and I couldn’t wait to introduce it to the world. After 19 minutes of pushing, Stella Hanoi gently slipped out into the water. Leopi carefully nudged her through my legs so that Josh could bring her up to me.
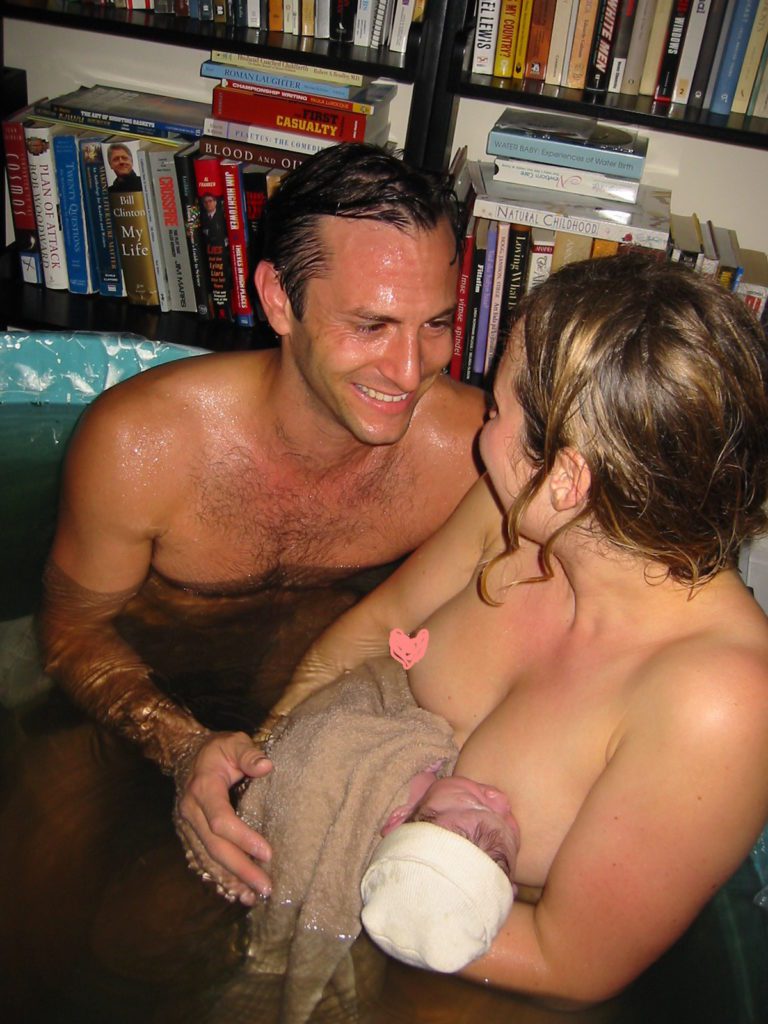
Stella looked curiously into our eyes. It felt as if I had always had her in my arms. After about 40 minutes Josh cut the cord and we went up. The midwives thought I was bleeding a little too much so they gave me a shot of synthetic oxytocin to stop the bleeding quicker. On my way into our bedroom I said that I wanted to do this at least 10 more times. Everyone laughed. In the light of a torch, Leopi gave me a few stitches since I had tore a little bit, probably because I had pushed so hard and fast. At last we got into bed and the midwives left quietly. The following day they came back to check on us and Stella. We stayed in bed for the rest of the week and were cared for by friends and family who came over with nutritious meals. That way we could spend all our energy on our little star.
In 2012 and 2015 I had two more amazing home births, in Sweden.
*I found studies showing that planned home births, for low risk women in countries where midwifery is part of the healthcare system, are associated with similar safety to low risk hospital births. They also showed that the rates for medical interventions for planned home births were lower than for low risk hospital births. The term low risk is applied to women who are healthy and carry a single baby.

About the Founders
Maria Bengtsson Lenn has previously worked as a journalist and doula, and is the author of two books on pregnancy and birth.
She has a Doula certificate from ODIS (Organisationen för doulor och Förlossningspedagoger i Sverige) and has trained with the well known doula trainer, childbirth educator and author Debra Pascali Bonaro, in her Advanced Birth Support Workshop.
Maria gave birth to her three children at home, with the support of her husband and wonderful midwives. She loves everything to do with empowering women, attachment parenting and happy babies. She believes this is the foundation for a more peaceful and healthy world.
Maria lives with her family on an island in the Stockholm archipelago.
Kristina Turner is a writer and birth activist with 25 years’ experience. She wrote the book Natural Birth – A Holistic Guide to Pregnancy, Childbirth and Breastfeeding after giving birth to her children at home.
The deeply transformative experiences she had during these undisturbed births led her to recognise that birth has the potential to be an initiatory experience for all women. This led her to her current work, which focuses on effecting structural change and giving more women the opportunity to have intact births. She is a vocal advocate of women’s birth rights and evidence-based maternity care.
Kristina is a certified Sacred Birthkeeper at Glastonbury Goddess Temple in the UK.
Kristina and Maria have worked together for many years to raise awareness around women’s rights in childbirth and to educate and inspire women to empower themselves.
Our acclaimed programs transform pain and fear into power and pleasure

For Parents
Ensure you are positively prepared for a safe, satisfying, and pleasurable birth and a loving, intimate relationship as a parent. From planning your unique birth experience to reconnecting with your sexuality after birth, our programs offer exactly what you need!
Our resources will empower you!
© Gwen Schroeder |Rebirth Photography

For Doulas
Be at the forefront of the new paradigm of birth as a sought-after doula, trained by one of the world’s most well-known leaders in pregnancy, birth, and postpartum. Our courses offer continuing education credit, mentorship, and inspiration to expand your practice with tools and tips for Orgasmic Birth and parenting with pleasure.
You’ve come to the right place!
© Monet Nicole

